Home | Evidence | Anatomy |
Imaging & Radiographs
IMAGING AND RADIOGRAPHS

This section is to help you understand the different
imaging and diagnostic options available to many practitioners today,
and help you with some idea about what you need to look for when understanding
your own images, scans and radiographs. There are many technologies available
today which can assist chiropractors in locating and correcting the source
of your discomfort. The scientific validity of these technologies is
not in question.
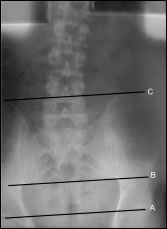
 X-ray: X-ray:
Scoliosis
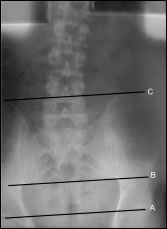
- This X-ray on the left was taken with the patient in standing position.
The X-ray equipment is calibrated to ensure accuracy. Line A; on
the X-ray shows the height of the two femurs to be the same. Therefore
the scoliosis is not related to an anatomical short leg. Atlas subluxation
pulls pelvis high on left. B and C are lines which indicate that
the pelvis has lifted. According to upper cervical chiropractic research
and case studies, this pelvis tilting occurs in compensation for
the atlas subluxation at the top of the cervical spine. |
 X-ray: X-ray:
Scoliosis - This X-ray on
the right was taken with the patient in standing position. The X-ray
equipment is calibrated to ensure accuracy. Line A; on the X-ray
shows the height of the two femurs to be different. This person has
an anatomical short leg (measured by CT scan to be 10mm or 0.4 inches).
Therefore the scoliosis shown here is related to this anatomical
short leg. B and C are lines which indicate that the pelvis has dropped
on the right, the side of the short leg. People who sustain an atlas
subluxation with an already short anatomical leg will incur further
scoliosis and pelvic distortion.
|
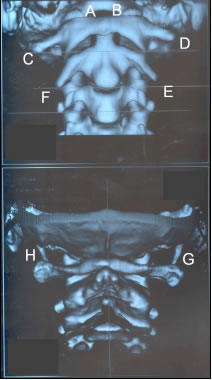 3
Dimensional Helical CT Scanner: 3
Dimensional Helical CT Scanner:
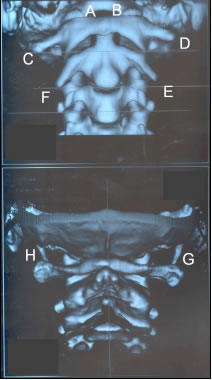
This is a 3D image (left)
of the upper cervical spine taken by a helical CT scanner. The
top scan
shows the cervical spine looking from the front of the patient
and the bottom is that from the rear. The CT scanner takes an
appropriate
number of slices and the software reconstructs those images into
the 3 dimensional scan shown opposite. Upper cervical chiropractic
(atlas orthogonal) vertex X-rays of this patient indicated an anterior
left subluxation of atlas to occiput. Interestingly, even though
these CT scans are taken with the patient lying down, this subluxation
would seem to be evident. You will note it appears that the right
occipital condyle (A) is more exposed than the left (B) and that
the atlas transverse process is more anterior on the left (D) than
the right (C). This is because the atlas has rotated forward on
the left. Further this person's head is tilted to the right due
to the
atlas subluxation. The weight of the head to the right causes a
widening of the gaps in the intravertebral foramen between C2
and C3 on the
left (E) and a reduction of the foramen on the right (F). What
happens to spinal nerves leaving the spinal canal through this
foramen? Could
one conclude that the spinal nerves leaving the canal at (E) would
be stretched by ligaments they travel through, and at the same
time compressed at (F)? Another indication of the altered weight
bearing
is the amount of the stylomandibular process which is shown. At
(G) there is more exposed than at (H). This is because the weight
of
the head is pushing the right transverse process of the atlas down
and the left up. That is, the atlas is not level with ground. A
combination of orthogonal and Blair upper cervical X-ray analysis
with some conventional imaging would, I think, reveal everything
about the articulations
in the upper cervical spine on most patients.
|
 2 Dimensional CT Scan: 2 Dimensional CT Scan:
This scan is another view of the same patient
in the 3D scan above. The scanning is from the bottom up, thus the
right side of these scans is actually the left side of the patient's
head. You will note in the bottom 3 scans that the atlas vertebra
is clearly rotated to the left anteriorly. If you look closely you
can see that the inner margins of the atlas vertebral ring appear
to overlap the foramen magnum (A).
 Radiologists considered the above CT scans to be "Within Normal Limits".
Could this actually be normal or is it the definitive signs of an upper cervical
subluxation? Blair upper cervical analysis would confirm whether or not this
person had offset occipital condyles (picture left), and thus whether or not
this anatomy was 'normal' for this patient. We wouldn't want to have our atlas
adjusted if this rotation was normal! Radiologists considered the above CT scans to be "Within Normal Limits".
Could this actually be normal or is it the definitive signs of an upper cervical
subluxation? Blair upper cervical analysis would confirm whether or not this
person had offset occipital condyles (picture left), and thus whether or not
this anatomy was 'normal' for this patient. We wouldn't want to have our atlas
adjusted if this rotation was normal!
"We must never forget that before any of us can know the correct
vertebral positions, we must first know of all existing asymmetries
and malformations." Dr. William G. Blair |
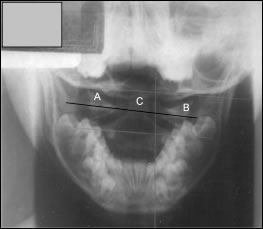 Nasium (open mouth) X-ray: Nasium (open mouth) X-ray:
This
is an X-ray of a 10 y.o. child. The atlas lateral masses are labeled
(A) and (B) and the odontoid process or peg is labeled (C). This
X-ray was taken with calibrated equipment and with the child standing,
and assuming her normal (for her) posture. Clearly the atlas is significantly
tilted and the centre line of the skull is not perpendicular to the
ground. Weight bearing on the cervical spine is now altered as the
head is off centre - "not on straight".
|
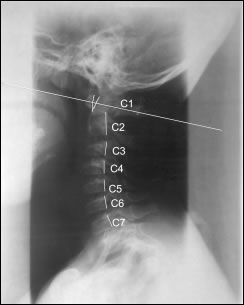
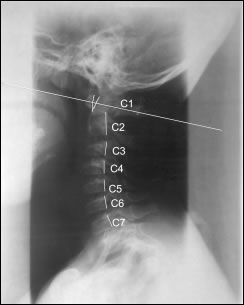 Now look at the effect of this altered weight bearing
on the normal (lordotic) curve of the cervical spine (right). I have
labeled the
cervical vertebrae and placed a line on the posterior portion of
the vertebral body. The head posture is forward, and you can see
that the gap between the anterior arch of the atlas and the dens
(odontoid process), indicated by the 'V' has widened. This is known
as the atlanto-dental interval (ADI) and when it widens and looks
like a 'V-sign' some authors suggest it indicates some instability,
whereas others suggest it could be due to congenital laxity of ligaments.
The loss of normal curve of the cervical spine which is occurring
at C2-C3 is due to the weight of the head and thus centre of gravity
now being forward of C7. A flattening out of the midline through
C1 as indicated by the white line is a further indication on altered
weight bearing of the skull on the cervical spine, manifesting itself
as observable forward head posture seen in many people today. The
radiologist report on the above X-rays included "Alignment of
the cervical spine is normal." You tell me if you think a child
who carries her head forward and with these X-rays has a 'normal'
cervical spine. Now look at the effect of this altered weight bearing
on the normal (lordotic) curve of the cervical spine (right). I have
labeled the
cervical vertebrae and placed a line on the posterior portion of
the vertebral body. The head posture is forward, and you can see
that the gap between the anterior arch of the atlas and the dens
(odontoid process), indicated by the 'V' has widened. This is known
as the atlanto-dental interval (ADI) and when it widens and looks
like a 'V-sign' some authors suggest it indicates some instability,
whereas others suggest it could be due to congenital laxity of ligaments.
The loss of normal curve of the cervical spine which is occurring
at C2-C3 is due to the weight of the head and thus centre of gravity
now being forward of C7. A flattening out of the midline through
C1 as indicated by the white line is a further indication on altered
weight bearing of the skull on the cervical spine, manifesting itself
as observable forward head posture seen in many people today. The
radiologist report on the above X-rays included "Alignment of
the cervical spine is normal." You tell me if you think a child
who carries her head forward and with these X-rays has a 'normal'
cervical spine.
|
"Atlas rotation following blow on the neck";
Australian Physician Magazine; Vol. 27, No. 6, June 1998,
'Letters to the Editor'; Pg. 461-62;
Drs F. Orenshaw and
P. Crooke of Healesville, Victoria, Australia.
I think it is appropriate here to digress slightly and make
reference to the 'Letters to the Editor' referred to above.
The letter discusses a woman who
received a blow to the neck from another player's elbow during a game of basketball.
Her symptoms shortly afterwards were "severe headache, nausea, giddiness,
a fainting sensation, pain in her neck and pins needles in her right hand." A
referral to cervical spine x-ray was reported as, "no abnormality is shown
in the cervical spine. The vertebrae are in normal alignment." The patient
referred herself to a chiropractor, who discussed the case with the doctors.
The chiropractor carried out manipulation to the upper cervical spine with
reported "dramatic results". Apparently, "Within 2 minutes facial
colour was restored, headache, nausea and dizziness were completely relieved".
Two days later further gentle chiropractic manipulation was done, which "relieved
residual neck pain and peripheral nerve symptoms". Drs Orenshaw and Crooke
raise the question of so called 'normal' X-ray findings with patients continuing
to suffer ongoing symptoms and finish with the comment "this case appears
to demonstrate the need for close scrutiny of upper cervical films to detect
quite small displacements of the atlas that can cause significant clinical
symptoms."
Those who are familiar with upper cervical subluxations
will know that what the two doctors refer to above is common
place in the community and is already known throughout the
chiropractic profession. These types of subluxations are
detectable on precision upper cervical chiropractic X-rays
and in most cases can be corrected by utilizing upper cervical
chiropractic techniques. It's time the medical profession
realized that many of their patients today actually have
these subluxations, and further they would most likely be
helped by referral to 'specific' upper cervical chiropractors.
The evidence linking upper cervical subluxations to myriad
conditions and symptoms is abundant. Likewise, the evidence
linking upper cervical chiropractic to correction of these
upper cervical subluxations and reversal of the associated
conditions and symptoms is also abundant. The above results
come as no surprise to those familiar with chiropractic.
The average medical doctor does not understand chiropractic.
The medical profession should engage upper cervical chiropractors
and work in unison with them to manage cases. Patients will
be the main beneficiaries. Isn't that what it's all about? |
|
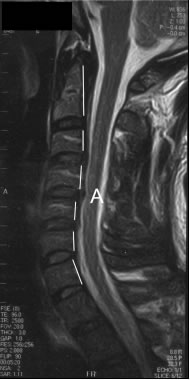 Magnetic
Resonance Imaging (MRI): Magnetic
Resonance Imaging (MRI):
Another type of imaging (left)
which can be used is MRI. The image to the left is that of the cervical
spine of the same person in the 3D and 2D CT scan above. You will
note the loss of cervical curve resulting from forward head posture.
The white lines again indicate the anterior ring of the spinal canal.
Normal lordosis has been lost. You will also note disc bulges into
the spinal canal impinging on the thecal sac. There is a small disc
bulge at C3/C4, a bigger one at C4/C5 (A) and a smaller one again
at C5/C6. Thus the altered weight bearing on the cervical spine,
due to the "head not being on straight" and not sitting
perpendicular atop the cervical spine, changes the biomechanics of
the cervical spine. This in turn, over time, causes the vertebral
bodies to compress down on the discs between them pushing the discs
into the spinal canal. Degenerative processes are at work and unless
addressed this type of situation becomes chronic. The head goes further
forward, muscles holding the head up become atrophic, vertebral fusion
processes progress and the symptoms (neurological, vascular and musculoskeletal)
associated with such spinal injuries increase in intensity.
|
 Electromyography
(EMG): Electromyography
(EMG):
Electromyography is the measurement of electrical activity that occurs within
muscle fibres in response to nervous system stimulation. As muscles contract
electrical signals with amplitudes in the microvolts (millionths of a volt)
range, are created within the muscles. Sensors placed on the skin's surface
detect these electrical signals and the active muscles and provide this information
to the EMG unit. In chiropractic EMG can be used to help locate muscles which
are 'tight' or in 'spasm'. Typically, this would be at the site of a subluxation.
Upper cervical subluxations can create scoliosis, thus the areas which might
show up in EMG analysis would be at the site of the scoliotic curves. EMG can
be used to measure before and after upper cervical adjustment muscular problems,
as shown in the print outs on the right. The top shows the positions of muscular
activity, which also coincided with the patient's areas of pain. These areas
also correlate with the patient's scoliotic spine. The bottom EMG output, which
was taken after upper cervical chiropractic adjustment to the atlas, shows
much improved EMG levels. According to Chiroweb.com: 'Paraspinal EMG Scanning:
A Viable Technology for Chiropractic',
http://www.chiroweb.com/archives/09/09/02.html
"Chiropractic
adjustments alter paraspinal EMG readings. Chiropractors have often observed
dramatic palpatory
changes in paraspinal muscles pre- and post-adjustment. Shambaugh conducted a
study where surface electrodes were used to measure paraspinal EMG activity before
and after chiropractic adjustment. This study was reported in JMPT, a refereed,
peer-reviewed journal. Shambaugh concluded: "Results of this study show
that significant changes in muscle electrical activity occur as a consequence
of adjusting." Similar findings were reported in a study conducted by the
osteopathic profession. Ellestad et al. found that paraspinal EMG activity decreased
in patients following osteopathic manipulation. Similar changes did not take
place in controls."
|
Digital Infrared Imaging
(DII):
Reprinted with permission from Dr. William C. Amalu, DC, DABCT, DIACT, FIACT
- Vice President and Research Director - International Upper Cervical Chiropractic
Association [IUCCA]. For further detail and list of the references see website http://www.pacificchiro.com
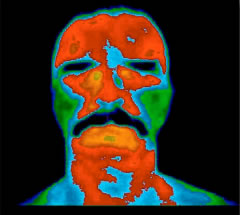 Over thirty years of clinical use and more than 8,000 peer-reviewed
studies in the medical literature have established digital infrared
imaging (DII) as a safe and effective means to examine the human
body. This highly specialized technology fills the gap left by less
sensitive procedures in determining a diagnosis. By assisting the
doctor in determining a diagnosis, DII ultimately helps to ensure
that a patient is receiving the most appropriate care for their condition. Over thirty years of clinical use and more than 8,000 peer-reviewed
studies in the medical literature have established digital infrared
imaging (DII) as a safe and effective means to examine the human
body. This highly specialized technology fills the gap left by less
sensitive procedures in determining a diagnosis. By assisting the
doctor in determining a diagnosis, DII ultimately helps to ensure
that a patient is receiving the most appropriate care for their condition.
DII is based on a careful measurement and analysis of skin surface
temperature. It is completely non-invasive and does not require
the use of radiation or
other potentially harmful elements. Special training is required to capture
as well as to interpret the images. Extensive research and investigation
performed at prestigious medical teaching institutions such as
Johns Hopkins University
Medical School, have established normal values for the distribution of heat
in each region of the body. During the DII examination, variation from these
normal values are measured and correlated with suspected injuries or diseases
in the same way a blood or urine laboratory study is interpreted.
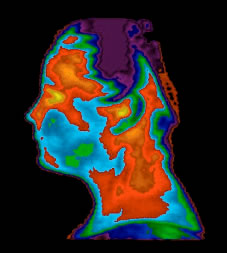 DII excels at measuring nervous system function. It possesses 96%
sensitivity and 94% specificity rating respectively. Sensitivity
is the ability to detect
an abnormal finding in a group of people known to have a particular condition.
Specificity is the ability to detect a normal finding in a group of people
known to be free of that condition. Other common imaging procedures such
as MRI, CT scan and EMG have ratings which are all under 90% and some possessing
up to 40% error ratings. In trying to measure the subtle nervous system
changes which accompany many injuries and disease states, use
of these other procedures
would be like trying to find a virus with a hand held magnifying glass. DII excels at measuring nervous system function. It possesses 96%
sensitivity and 94% specificity rating respectively. Sensitivity
is the ability to detect
an abnormal finding in a group of people known to have a particular condition.
Specificity is the ability to detect a normal finding in a group of people
known to be free of that condition. Other common imaging procedures such
as MRI, CT scan and EMG have ratings which are all under 90% and some possessing
up to 40% error ratings. In trying to measure the subtle nervous system
changes which accompany many injuries and disease states, use
of these other procedures
would be like trying to find a virus with a hand held magnifying glass.
Many imaging procedures demonstrate changes in the structure of
the body (anatomy) but do not measure how well it functions (physiology).
X-ray,
CT scan, and
MRI all look at anatomy whereas DII measures physiology. The use of anatomical
imaging exclusively to detect a nerve problem would be incomplete. This
would be similar to a mechanic trying to diagnose a car problem by looking
at all
the parts of the vehicle and never hooking it up to an analyzer and turning
the car on.
Digital Infrared Imaging is not limited to the detection of nervous
system conditions. Medical research has shown it to be helpful
in the diagnosis
of, Breast Cancer, Repetitive Strain Injuries, Headaches, Neck and
Back Problems, TMJ Conditions, Numerous Pain Syndromes, Arthritis,
Vascular
Disorders, and
Soft Tissue Injuries among others. Treatment failure is often the result
of
incomplete or misdiagnosis. By assisting the doctor in determining
the diagnosis, DII ultimately helps to ensure that a patient
is receiving
the most appropriate
care for their condition. |
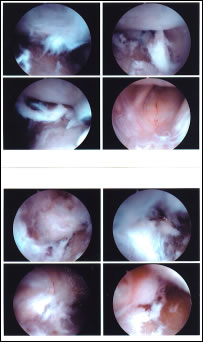
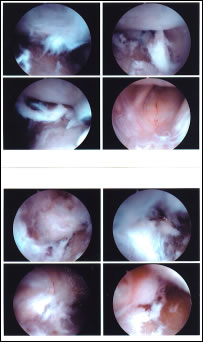 Arthroscope: Arthroscope:
Although not a diagnostic procedure used by chiropractors,
the images (left) being arthroscopic pictures showing right and left
temporomandibular joints (TMJ), are interesting because they are
of a patient who sustained an upper cervical subluxation and was
reporting noises in the right jaw joints soon after. The patient's
head tilt was to the right and it is the right TMJ (bottom) which
shows most damage to the meniscus (cartilage) which lies between
the jaw (mandible) condyle and the skull socket (fossa). Upper cervical
subluxations which cause the patient's head to move off centre, thus
resulting in head tilt, can result in the misalignment of the TMJ
condyle into the socket in the skull. This misalignment or incorrect
articulation of the joints causes the jaw condyles to 'catch' the
meniscus during normal jaw movement as with eating, talking and yawning.
This 'catching' can result in tearing of the meniscus and ongoing
damage to the TMJ mechanism. TMJ symptoms as reported by patients
of TMJ physicians or dentists correlate highly with those symptoms
reported by upper cervical chiropractic patients. TMJ symptoms have
been shown to resolve following upper cervical chiropractic adjustment
and also following TMJ dentistry. Some dental physicians also report
resolution of patients' poor posture following TMJ dentistry, and
certainly poor posture is rectified following upper cervical chiropractic
adjustment.
|
SUMMARY:
It can be shown that there are many imaging options available to
today's practitioners. In my experience it is also patently obvious
that much pathology is 'missed' and people complaining of what eventually
become chronic symptoms are never really helped in a timely manner.
Upper cervical chiropractors are trained in detecting sometimes subtle
signs in their patients' cervical spines; usually after the patient's
standard radiographs have been classed as 'normal' or 'within normal
limits'. I find time and time again that main stream medical practitioners
dismiss out of hand findings on radiographs made by experienced chiropractors.
I think it's time to concede that chiropractic examination, which
has been around for decades, does provide appropriate methodologies
to reveal 'hidden' or 'missed' pathologies. It can then be hypothesized
that these pathologies do lead to chronic symptoms and as evidenced
by chiropractic cases and studies, such symptoms may be reversed
with chiropractic intervention. It also highlights how important
it is for chiropractors to utilize 'specific', that is 'precision',
upper cervical analysis and adjustment techniques.
I think that the following study shows just how important it is
to have an open mind and to be alert when examining cervical spine
imaging of patients who have been involved in some kind of accident
involving a direct head injury (of any force) or whiplash event.
Comparison of Radiographic, MR Imaging, Anatomic, and Pathologic
Findings Radiology, November, 2001;221:340-346.
Authors: Axel Stäbler, MD, Jurik Eck, MD, Randolph Penning,
MD, Stefan P. Milz, MD, Reiner Bartl, MD, Donald Resnick, MD and
Maximilian Reiser, MD
In this study the cervical spines of 10 accident victims were examined
using radiography and MR imaging. The results indicated that radiographic
X-rays found only 4% of lesions and that only 11 of 28 lesions were
found using MRI. Soft tissue injuries accounted for 89% of c-spine
lesions detected in postmortem images and some factures were missed
by X-rays. The authors note that "the c-spine is a particularly
susceptible site for injury" and these "injuries are often
occult." A further study involving 22 traffic accident victims
found 245 various lesions which "were not detected on radiographs."
Other notes by the authors are; "Hyperextension
injuries of the cervical spine are common and are associated with
a risk of spinal
cord compromise of variable degree even in the presence of normal
radiographs." And "hyperextension injuries... often show
only subtle radiographic abnormalities, even in severe and unstable
lesions." The
study confirms "the high frequency of associated cervical spine
injuries after severe head injuries."
DOWNLOAD
PDF |
(requires Adobe Acobat
Reader) |
img_rad.pdf
(395kb) |
|
|
|
|




 Radiologists considered the above CT scans to be "Within Normal Limits".
Could this actually be normal or is it the definitive signs of an upper cervical
subluxation? Blair upper cervical analysis would confirm whether or not this
person had offset occipital condyles (picture left), and thus whether or not
this anatomy was 'normal' for this patient. We wouldn't want to have our atlas
adjusted if this rotation was normal!
Radiologists considered the above CT scans to be "Within Normal Limits".
Could this actually be normal or is it the definitive signs of an upper cervical
subluxation? Blair upper cervical analysis would confirm whether or not this
person had offset occipital condyles (picture left), and thus whether or not
this anatomy was 'normal' for this patient. We wouldn't want to have our atlas
adjusted if this rotation was normal!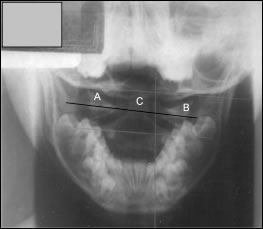
 Now look at the effect of this altered weight bearing
on the normal (lordotic) curve of the cervical spine (right). I have
labeled the
cervical vertebrae and placed a line on the posterior portion of
the vertebral body. The head posture is forward, and you can see
that the gap between the anterior arch of the atlas and the dens
(odontoid process), indicated by the 'V' has widened. This is known
as the atlanto-dental interval (ADI) and when it widens and looks
like a 'V-sign' some authors suggest it indicates some instability,
whereas others suggest it could be due to congenital laxity of ligaments.
The loss of normal curve of the cervical spine which is occurring
at C2-C3 is due to the weight of the head and thus centre of gravity
now being forward of C7. A flattening out of the midline through
C1 as indicated by the white line is a further indication on altered
weight bearing of the skull on the cervical spine, manifesting itself
as observable forward head posture seen in many people today. The
radiologist report on the above X-rays included "Alignment of
the cervical spine is normal." You tell me if you think a child
who carries her head forward and with these X-rays has a 'normal'
cervical spine.
Now look at the effect of this altered weight bearing
on the normal (lordotic) curve of the cervical spine (right). I have
labeled the
cervical vertebrae and placed a line on the posterior portion of
the vertebral body. The head posture is forward, and you can see
that the gap between the anterior arch of the atlas and the dens
(odontoid process), indicated by the 'V' has widened. This is known
as the atlanto-dental interval (ADI) and when it widens and looks
like a 'V-sign' some authors suggest it indicates some instability,
whereas others suggest it could be due to congenital laxity of ligaments.
The loss of normal curve of the cervical spine which is occurring
at C2-C3 is due to the weight of the head and thus centre of gravity
now being forward of C7. A flattening out of the midline through
C1 as indicated by the white line is a further indication on altered
weight bearing of the skull on the cervical spine, manifesting itself
as observable forward head posture seen in many people today. The
radiologist report on the above X-rays included "Alignment of
the cervical spine is normal." You tell me if you think a child
who carries her head forward and with these X-rays has a 'normal'
cervical spine. 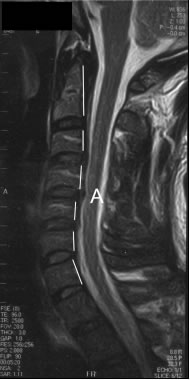 Magnetic
Resonance Imaging (MRI):
Magnetic
Resonance Imaging (MRI):  Electromyography
(EMG):
Electromyography
(EMG):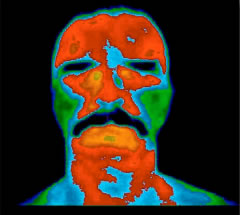 Over thirty years of clinical use and more than 8,000 peer-reviewed
studies in the medical literature have established digital infrared
imaging (DII) as a safe and effective means to examine the human
body. This highly specialized technology fills the gap left by less
sensitive procedures in determining a diagnosis. By assisting the
doctor in determining a diagnosis, DII ultimately helps to ensure
that a patient is receiving the most appropriate care for their condition.
Over thirty years of clinical use and more than 8,000 peer-reviewed
studies in the medical literature have established digital infrared
imaging (DII) as a safe and effective means to examine the human
body. This highly specialized technology fills the gap left by less
sensitive procedures in determining a diagnosis. By assisting the
doctor in determining a diagnosis, DII ultimately helps to ensure
that a patient is receiving the most appropriate care for their condition.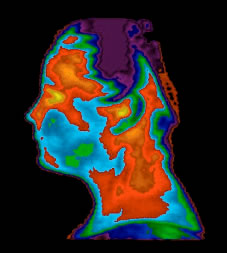 DII excels at measuring nervous system function. It possesses 96%
sensitivity and 94% specificity rating respectively. Sensitivity
is the ability to detect
an abnormal finding in a group of people known to have a particular condition.
Specificity is the ability to detect a normal finding in a group of people
known to be free of that condition. Other common imaging procedures such
as MRI, CT scan and EMG have ratings which are all under 90% and some possessing
up to 40% error ratings. In trying to measure the subtle nervous system
changes which accompany many injuries and disease states, use
of these other procedures
would be like trying to find a virus with a hand held magnifying glass.
DII excels at measuring nervous system function. It possesses 96%
sensitivity and 94% specificity rating respectively. Sensitivity
is the ability to detect
an abnormal finding in a group of people known to have a particular condition.
Specificity is the ability to detect a normal finding in a group of people
known to be free of that condition. Other common imaging procedures such
as MRI, CT scan and EMG have ratings which are all under 90% and some possessing
up to 40% error ratings. In trying to measure the subtle nervous system
changes which accompany many injuries and disease states, use
of these other procedures
would be like trying to find a virus with a hand held magnifying glass.